Lumbar Disc Prolapse & Radiculopathy - Fact Sheet
What is a Lumbar Disc Prolapse & Radiculopathy ?
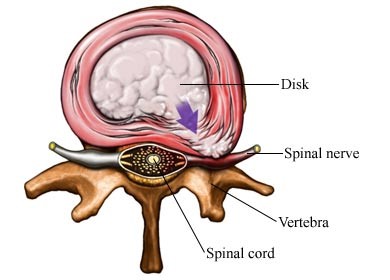
The spine is made up of linked segments of bone called vertebrae. In between each vertebra is a ‘spongy’ disc. The disc consists of a central sac of fluid the ‘nucleus’, surrounded by a layered ring of ligaments the ‘annulus’. The disc acts as a cushion for your spine, as well as allowing movement between each segment to provide the spine with flexibility. A disc prolapse occurs when the fluid of the nucleus protrudes through the annulus, so that that it is no longer contained within the annular ligaments. This fluid can “impinge” the exiting nerve roots of the spine, causing a radiculopathy.
How does it happen?
A number of issues can contribute to a prolapse, which could include
• Prolonged sitting and or poor posture – Can degrade the annulus over time
• Poor lifting technique – Increases the pressure inside the disc and pushes the nucleus back against the ligaments
• Muscular weakness and poor core stability – Will expose the spine to an increased amount of stress which may cause the rupture.
Signs and Symptoms of a Lumbar Disc Prolapse ?
• Significant localised back pain
• Severe lumbar disc prolapses can have the following associated symptoms: Nerve pain (burning, shooting pain) down the legs; “pins and needles” down the legs; numbness of particular muscles or areas of the skin; significant weakness of lower limb muscle groups; & loss of, or hypersensitised, lower limb reflexes. When 2 or more of these symptoms are present, this is termed a radiculopathy.
• Go to the hospital immediately if your low back pain is associated with: pain with walking (claudication); numbness/pins and needles of the “saddle” area – the coccyx and perineum; &/OR difficulty and pain with initiating bladder or bowel movements.
Diagnosis & Investigations
• A Physiotherapist, Osteopath or Accredited Exercise Physiologist can help diagnose a lumbar disc prolapse and/or radiculopathy via thorough lumbar spine and nervous system clinical and mechanical testing.
• An MRI can help figure out the extent of the disc prolapse, what levels of the spine are affected, and whether or not there is involvement of the exiting nerve roots.
• Depending on the severity of symptoms, a consult with a specialist neurologist may be considered.
.
.


Treatment of Lumbar Disc Prolapse & Radiculopathy ?
Hands on treatment: techniques such as traction can help reduce the pressure on the spine and nerve roots, helping “centralise” and lower leg symptoms back to the spine. This, combined with tolerable movements of the spine, can relocate any disrupted disc fluid back into the centre of the disc. This should not be solely relied upon to reduce pain, as evidence suggests this works best in conjunction with specific, individualised exercise programming.
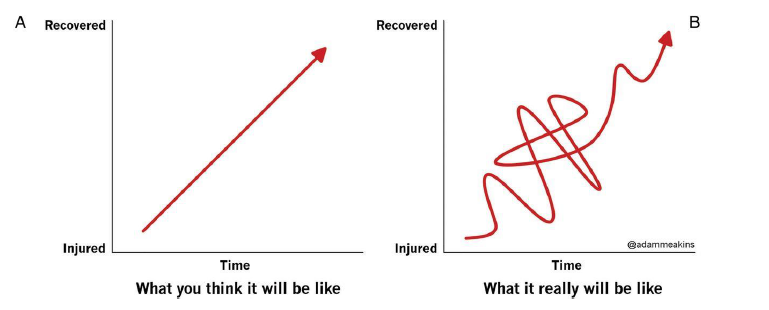
Tailored Clinical Exercise will help to strengthen the core muscles that support your spine (including your deep abdominals, lumbar erector muscles, and gluteals/buttocks), thus helping centralise your symptoms and decrease the severity your pain. Disc prolapses can be re-absorbed and fully recovered with clinical exercise alone!!! Because of this, exercise can be considered the first-line treatment for a disc prolapse. Patience is the key with rehab for a disc prolapse, as it can take anywhere from 3 to 18months to have improvements in symptoms, sometimes even longer for a full recovery!
Surgical options: depending on severity, a surgery called a discectomy +/- a lumbar fusion may be an option. However, because of all the sensitive structures around the lumbar spine, surgeries can have significant risks, so this should be considered a last resort of treatment. Other things that may be considered to reduce symptoms is corticosteroid injections into the nerve root, which may/may not be effective.
Other things to be aware of:
Be aware of your posture: Poor posture can be a precursor to discogenic pain. Avoid sitting with a bent back for long periods. Try and sit upright. A lumbar support in the form of a rolled-up towel resting in your lower back may also be useful, when driving or sitting for long periods.
Lifting: Try and limit the amount of lifting you have to do. If you must, lift the load close to the body, keeping your back straight. Remember to bend your knees and use your leg muscles.
Take medication: During acute flare ups, painkillers and anti-inflammatories can help control the severity of your symptoms. Ask your doctor or pharmacist what medication is right for you and be aware of possible side effects. In severe cases, medication can control the pain so that physical activity can begin.
Flare ups: Re-occurrences of discogenic low back pain often occur, but it is important to remember that this is a normal part of the recovery process. Complete rest (such as bed rest is NEVER the answer – keep moving, keep positive – your symptoms will eventually settle down.