Greater Trochanteric Pain Syndrome (GTPS ) (Including gluteal tendinopathy) - Fact Sheet
What is a Greater Trochanteric Pain Syndrome (GTPS) (Including gluteal tendinopathy) ?
Greater Trochanteric Pain Syndrome (or GTPS) is an umbrella term for a range of conditions causing pain in the lateral hip. This includes conditions such as trochanteric bursitis, and gluteal tendinopathy. The exercise-based treatment for these conditions is very similar.
What is gluteal tendinopathy?
Gluteal tendinopathy is generally thought to be caused by improper or excessive load on the gluteus minimus and/or medius tendons, leading to pain with use/load. The tendons’ fibre can become disarrayed and therefore can lose their regular load-bearing capacity. Pain is generally felt with pressure on the tendon itself on the lateral hip, and in the gluteus medius muscle belly (closer to the middle of the buttock). Pain for this issue is proportionate to load or activity – if the load or activity exceeds the current capacity of the tendon(s), this leads to pain either during or following the activity. Pain is generally worse in the morning upon rising from bed, as the tendon hasn’t “warmed up” yet.
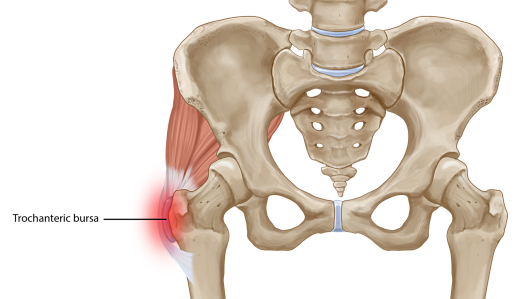
What is trochanteric hip bursitis?
The greater trochanteric bursa is a small sac of fluid which acts as a lubricant for the tendons of the lateral hip over the thigh bone (femur). If this structure is irritated, it can become inflamed, leading to bursitis. This can cause pain locally at the greater trochanter (the bony part of the lateral hip), or refer pain down the lateral thigh. As this is an inflammatory issue, pain is generally worse at night, and can be painful to sleep on that hip as it causes direct pressure on the bursa.
.
Factors that can contribute to GTPS ?
• Poor gluteal strength and capacity to tolerate load
• Being overweight
• Rushing headfirst into a full-on exercise program, without gradually building exercise capacity.
• Direct falls or blows to the lateral hip
• Poor exercise technique or biomechanical faults
• Prolonged sitting
.

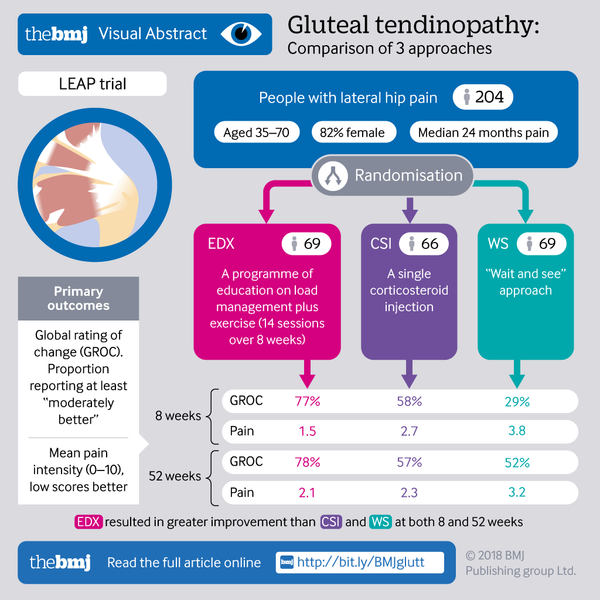
Treatment of Greater Trochanteric Pain Syndrome ?
Activity modification – Reducing or modifying any aggravating activities or exercises. As a general rule, pain shouldn’t be higher than 3-4 out of 10 either during or after any given activity or exercise. If this is higher, the load/intensity of this exercise needs to be reduced.
Abduction ISOs – Isometrics, or ISOs of the lateral hip muscles can help gradually build-up load capacity again with low risk of re-injury or pain flare-ups. In fact, ISOs can also have an analgesic effect on the lateral hip, reducing pain immediately after the exercise. An Exercise Physiologist or Physiotherapist can help guide you on the correct dosage and intensity of your ISO exercises.
Gradual return to full activity – As pain permits, slow re-introduction into full muscle contractions of the lateral hip muscles, with a focus on technique. Again, pain levels should not rise to higher than 3 or 4 out of 10 when these types of exercises get introduced. Once these are more tolerable, a gradual return to full activity can start to occur. If you are returning to sport, introduction of plyometric (jumping and landing) exercises is strongly recommended.

Other things to be aware of?
Avoid compression and stretching – a tightness feeling can occur in the lateral hip when you have GTPS. If this happens, avoid stretching the area, as the tendons and bursa DO NOT tolerate stretching well! Instead, try some ISOs. Avoid compression of the area too – sitting with legs crossed, sitting with hips flexed past 90degrees, and long periods of sitting can aggravate this issue.
Injections – for bursitis only, guided corticosteroid injections can be indicated if the hip pain doesn’t improve after a period of exercise-based treatment. Keep in mind though – injections only mask pain, so exercise is still paramount to build up the capacity of the lateral hip to tolerate loads again.